Children and adolescents are known to be very active and undergo regular growth spurts. These sudden changes in height and increasing load on their joints can increase the chance of developing pain and injury. As the Winter sport’s season commences, we see many children presenting with aches and pains.
Firstly, an important point on growing pains:
What are growing pains? Growing pains are an extremely common condition experienced by children and adolescents. This pain typically presents behind the knees, in the calves and in the thighs. They can also affect other joints such as the elbow.
Growing pains are simply generalised muscular pain, caused by the muscles stretching as the bones lengthen during growth. The pain is usually on both sides of the body, increases in severity in the afternoon and evening, and often disrupts sleep. There is no physiological damage being caused to the muscles or bones as a result of growing pain, however the discomfort can be quite severe.
How do I know if my child’s pain is more than just growing pains? If you child is experiencing pain that is unilateral or in one limb, has pain in the morning, or swelling and redness, you should consult a health professional (GP or physiotherapist).
The following three disorders are examples of common conditions (that are more than just growing pains) that children and adolescents can develop. These do need to be assessed and treated by a medial professional to prevent serious complications and minimise downtime from activities.
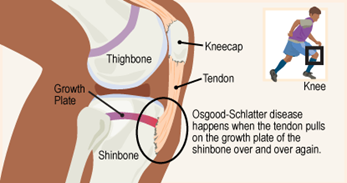
Osgood-Schlatter’s Disease (OSD)
A common cause of knee pain in kids that occurs when the patella tendon that attaches the quadriceps muscle to the tibia becomes tight and pulls on its bony insertion. OSD is most common during puberty and large growth spurts. It mainly affects active kids who play jumping sports where repetitive use of the quadriceps is required eg: basketball, netball, football and soccer. It is common to feel an excess bone formation at this insertion.
Treatment:
- Load management and activity modification to allow healing
- Biomechanical assessment to reduce the load on the quadriceps
- Rehabilitation exercises
- Wearing supportive shoes.
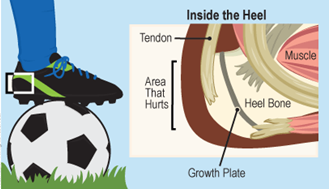
Sever’s Disease
Similar to OSD, Sever’s disease presents as pain and swelling where the Achilles tendon attaches the calf muscle to the calcaneus (heel). During a growth spurt, the bones, muscles, and tendons all grow at different rates. This can lead to the muscles and tendons tightening and pulling on the bony attachment of the Achilles. This condition is also prominent in running, hopping and jumping sports and in kids who are very active. Pain is usually worse during or after activity and can cause limping.
Treatment
- Biomechanical assessment to reduce the load on the calves
- Load management and activity modification to allow healing
- Podiatry review, or trial orthotics to improve foot mechanics
- Avoid over stretching
- Rehabilitation exercises
- Wearing supportive shoes
- Ice post exercise/activity
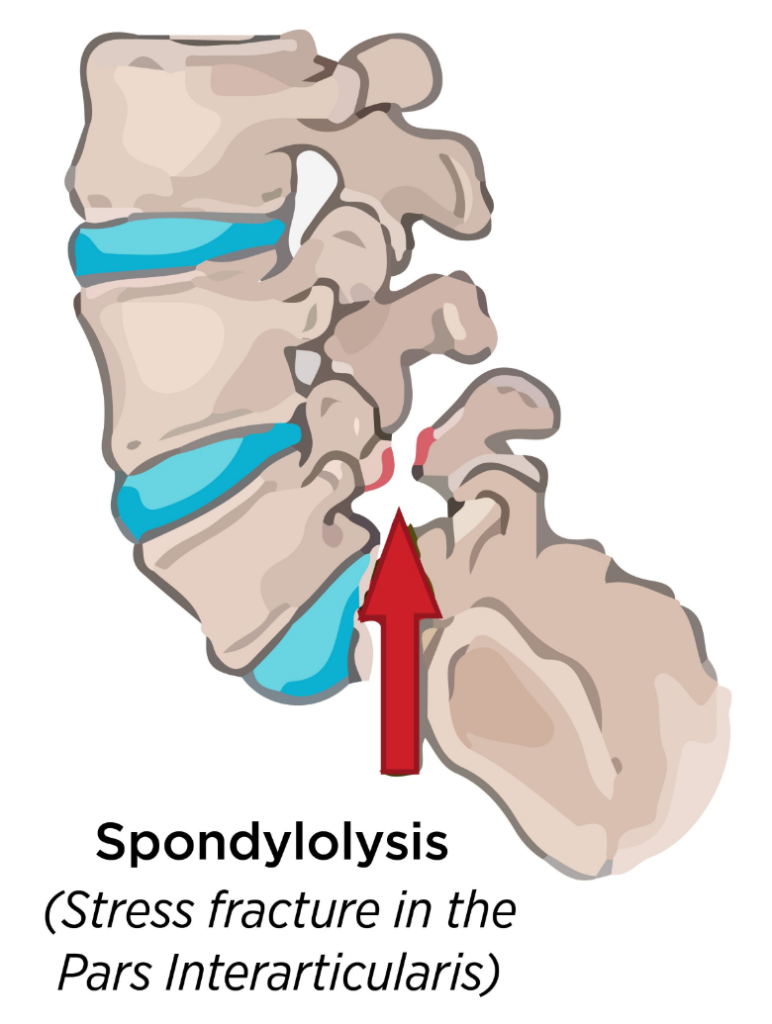
Spondylolysis (Pars Defect)
A Pars defect is a stress fracture that develops in a section of the vertebrae in the spine. Unilateral back pain is the main complaint however leg pain and muscle spasm can also be reported. Typically, a pars defect is associated with sports that require repeated back extension (leaning backwards) eg: cricket, gymnastics, dancing and football. Pars defects most commonly occur due to a sudden increase in intensity and frequency of training or competitions, as a result of the spine being overloaded. Early diagnosis is essential to avoid longstanding issues.
Treatment:
- Load management, activity modification and avoiding aggravating sports until defect has healed
- Biomechanical assessment and graded rehabilitation exercises under physio guidance
- Good backpack posture
- Massage based treatment
Please note that this is a guide only to help manage the conditions once your child has received a diagnosis. If you are worried that your child may be experiencing one of these conditions, please book into your physiotherapist, GP or sport’s physician for an assessment.
